Two years ago, in the early days of a novel coronavirus spreading methodically to almost every corner of the planet, it was something of a race. The planet’s best scientists were trying to keep up.
“When the pandemic started, one of the things that became eminently clear was that we were way too slow at diagnosing it and determining if somebody had COVID-19,” says Neal Woodbury, vice president of research and chief science and technology officer with Arizona State University’s Knowledge Enterprise.
In the pandemic’s early months, health care in the U.S. and other nations had stumbled over the scale, speed and accuracy of testing for the virus.
“And we all realized that there wasn't going to be one set of solutions. You weren't going to solve this one way,” says Woodbury.
Testing for the virus — especially prior to vaccinations being available — was a key component in containing it.
The “magic-wand wish” was for “point-of-need” testing: simple, fast, cheap and reliable testing tools that could be put to use in crowded places like airports, theaters, concerts — anywhere people might gather quickly in large numbers.
Scientists within ASU pulled together a huddle to share ideas.
“What we wanted to accomplish was to create tests that allow people to detect early infection so that when they gather, they can gather with confidence that they're not going to be in an environment where there's potential transmission,” says Jennifer Blain Christen, who leads ASU’s BioElectrical Systems and Technology group.
It was a tall order. Biotech firms, government health agencies and universities around the world have been running together in this marathon for more than two years. ASU’s group won strong financial support from Arizona’s Department of Health Services in September 2020. The money has been put to work in three silos of virus testing innovation.
Blain Christen is an electrical engineer. She and her team now have working prototypes of test machines that would be small and portable. They begin with a small amount of saliva, which is pressed through a flat plastic cassette. Wells in the cassette pull the saliva into chemical reactions. Within minutes, a scanner reads the outcomes as positive, negative or in error. Picture the device inside a doctor’s office, or at the entrance of a large meeting.
“We could simply ask them to come about 40 minutes early, provide a saliva sample and have very high-quality testing that detects early infection,” says Blain Christen, an associate professor in the Ira A. Fulton Schools of Engineering. “Before you have any symptoms, before an antigen test would be effective, we can detect those early indicators of COVID-19. And that allows people to gather, and they'll be in a safe environment.”
Work continues to make the devices even smaller, more streamlined and modular.
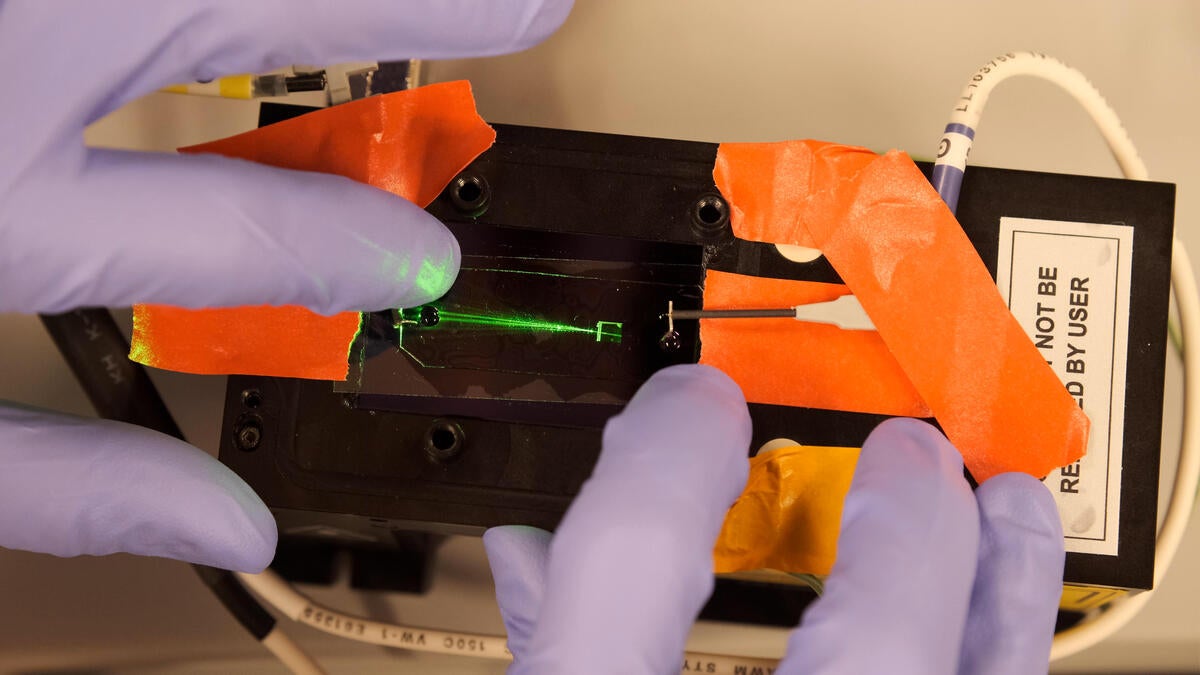
Mark Hayes is a molecular scientist. He and his team have poured their efforts into solving the testing problem through what’s called microfluidics. Think of it as sorting viruses and particles through flat, clear plastic slides, then hitting them with lasers and electrical currents. Hayes explains the big idea with a familiar image: the gigantic beam of light that shines from the Luxor hotel's pyramid in Las Vegas.
“You can see individual insects flying around in that beam of light,” says Hayes, a professor in the School of Molecular Sciences. “And it's a similar idea here. We have a little microfluidic device; we're shooting a laser on it. If there's a particle there — we filter out everything else but the coronavirus particle — it'll scatter a little bit of light, and we can pick that up on our cameras.”
Chips for sorting the virus particles could be made inexpensively and on a massive scale.
Alex Green is a biomedical engineer, now at Boston University’s College of Engineering. Green and his team drove new work in lab-ready diagnostic tests. Their role was converting an assay he had developed for the Zika virus to work for SARS-CoV-2, which became the “reader” for the devices.
“Basically, you want to have the ability to do the tests in a very efficient manner, and be able to handle up to 10,000 tests per day, with high accuracy,” Green says. “For instance, this could be used in situations where you want to test students in a particular school district or where you’re serving the needs of a large community of people and need to understand the status of the virus inside that population.”
Each of the three efforts will need to pass review and testing by agencies like the U.S. Food and Drug Administration before they can emerge as products we’ll see out in the world, in places like testing labs, medical offices, airports or sports venues. That will probably take at least a year. But from the start, the ASU team was determined that their efforts would go beyond the labs of academia.
“All of these projects had to have a pathway to utilization,” says Woodbury. “In other words, it wasn't, ‘We're going to do some cool stuff and write a paper.’ That was not our objective. We were going to set them each up so that they could be commercialized and move out into the world. And I'm happy to say that each of them has a company path associated with them.”
ASU scientists did the research. Three companies are now carrying forward these efforts to commercialization:
- EN CARTA Diagnostics, where Alex Green is a strategic adviser: https://www.encarta.bio.
- Hayes Lab, led by Mark Hayes: https://sites.google.com/view/hayeslab.
- Flex Bio Systems and Tech, co-founded by Jennifer Blain Christen: https://flexbiotech.com.
Top image: A microfluidics device using beams of light to identify whether coronavirus particles are present.
More Health and medicine

Dynamic data duo advances health research
The latest health research promises futuristic treatments, from cancer vaccines to bioengineered organs for transplants to medical nanobots. While these technologies may one day be…

New study reveals high levels of toxins in seized cannabis from Arizona and California
A recent study conducted by researchers from Arizona State University has uncovered alarming levels of Fusarium mycotoxins in illicit cannabis samples seized in Arizona and California.The study found…

PhD student builds bridges with construction industry to prevent heat-related illnesses
It is no secret that Arizona State University has innovative researchers working to help solve everyday problems.According to a new preliminary report issued by Maricopa County, there were more…