As International Women in Engineering Day on June 23 approaches, two female biomedical engineering students at Arizona State University are preparing to debut a biomedical device on a world stage in London.
Mariam El Sheikha and Kelsey Boos are members of one of three ASU engineering teams headed to London this summer to advance their projects during the PLuS Engineering Summer School, then present them at an international showcase event. Their device is designed to speed upper limb function recovery for stroke patients.
Mariam El Sheikha
El Sheikha and Boos are traveling the course to medical school by way of biomedical engineering degrees — when they’re not preparing for their trip to London this summer, they are studying for their Medical College Admission Tests. Their project, the design and initial development of a therapeutic medical device that enhances physical therapy for stroke victims, serves as the perfect gateway between biomedical engineering and medicine.
El Sheikha was drawn to the biomedical path, and particularly this project, because of her grandfather. When he suffered a stroke in Egypt, “not only did he not have access to the biomedical devices we have in the U.S., he didn’t have access to comprehensive physical therapy,” El Sheikha said. “I wanted to do something that will help people’s lives.”
Kelsey Boos has always wanted go to medical school, and while she initially thought she would focus on pediatrics, her experiences in biomed have her considering an alternative path. Her roommates have careers as biomedical engineers who design and develop medical devices. “I can see myself working in those environments,” she said.
The women were part of a bioengineering interdisciplinary product development team (IPDT) for a class focused on the fundamentals of developing and bringing to market a biomedical device using best industry practices and an entrepreneurial mindset, including ethics, FDA regulatory processes and business practices.
The team assignment was based on a relatively new stroke therapy that uses a surgically implanted vagus nerve stimulation (VNS) device to enhance physical therapy after stroke. According to recent studies, VNS in concert with therapy can as much as double upper limb function recovery.
The students will present their project this July during the PLuS Engineering Summer School Showcase. Photo by Deanna Dent/ASU Now
“When stroke causes damage to the brain, repetitive physical therapy supports neural plasticity — a reorganization of neural circuits which, over time, assigns lost functions to new pathways and ultimately improves motor function,” explained Jeffrey Kleim, a Ira A. Fulton Schools of Engineering associate professor of biological and health systems engineering who conducts neuroplasticity research and is one of the course instructors.
“For example, when a patient tries to grasp an object, the old neural pathways no longer effectively connect to that action. VNS provides much needed extra neurotransmitters that drive neural plasticity to help reorganize brain function,” Kleim said.
“This promising clinical trial research result may be more practically translated in the clinic, and especially at the point-of-care, if a technology can be developed that allows the patient to self-direct (at home) therapy in addition to clinical guidance,” explained Vincent Pizziconi, an associate professor of biological and health systems engineering and director of the bioengineering design center. Pizziconi also is a course instructor.
Kelsey Boos
The challenge presented to the BME design class was to develop a low cost, noninvasive (nonsurgical), self-directed device that would facilitate at-home VNS therapy for stroke patients that would speed recovery and function — while reducing treatment costs and minimizing adverse events associated with implantable VNS devices.
In addition, a key product specification required for home use involved an ergonomic, or human factor consideration, such as ease of use.
The resulting, external device stimulates the vagus nerve through its auricular branch, which is located in the ear. In addition to triggering additional neurotransmitters, “there’s a closed feedback loop that ensures the patient is performing the motion correctly,” El Sheikha said. “The nerve is stimulated only during the correct therapeutic movements.”
The device itself mimics current earpiece models and is positioned in a way that won’t be displaced by movement or impede physical therapy. A built-in motion detector is used to signal the stimulation electrode.
The IPDT of 20 students was divided into four core technology groups: circuits, electrodes, microprocessor and systems integration.
El Sheikha, a member of the electrodes design team, developed the electrode circuit design for the earpiece. Boos, the section leader for systems integration team, designed an earpiece that accurately targeted the auricular branch of the vagus nerve for stimulation, while also guiding her team in the integration of Xbox Kinect technology.
According to Pizziconi, the novel concept of using Kinect technology has the potential to set the project apart from other medtech competitors.
“It was a valuable learning process to see that it could be done with multiple groups of people,” Boos said about the process that had teammates working in their assigned areas before coming together to integrate all of the components.
For El Sheikha, the process has been an opportunity to familiarize herself with tools she’ll be using as a physician. “As a doctor, it’s important to investigate how you can improve a device and provide feedback to the technology developers,” she said.
Both women are looking forward to sharing the project in London and getting feedback from international perspectives.
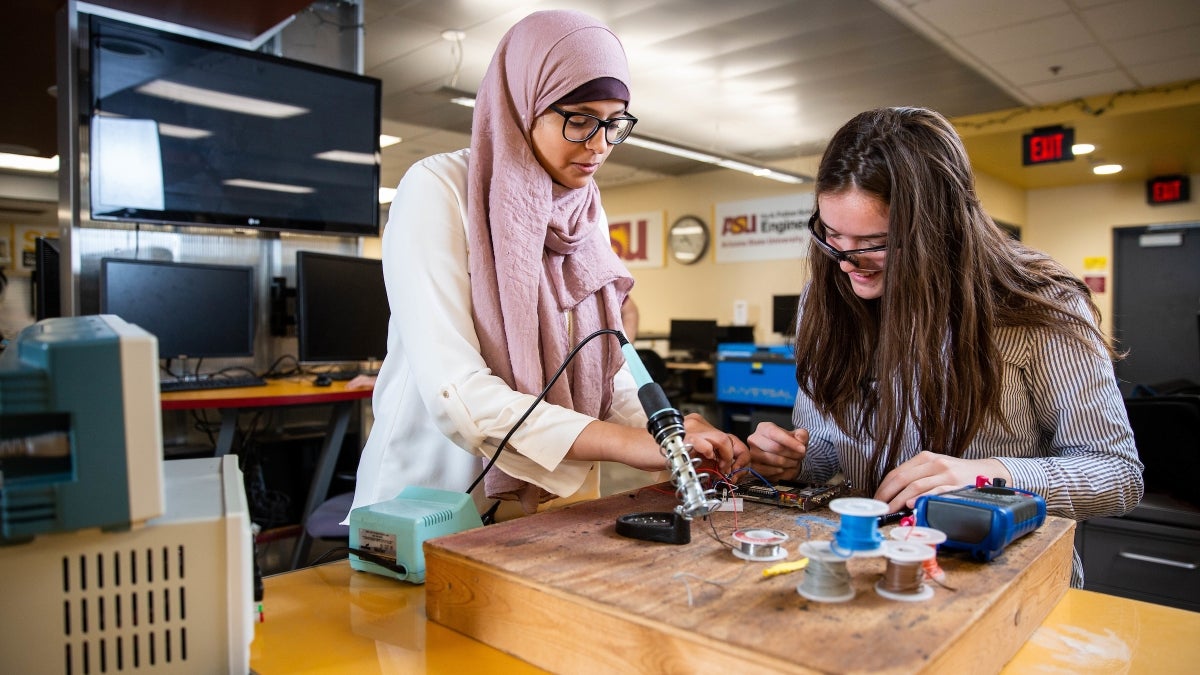
Top photo: Mariam El Sheikha and Kelsey Boos work on the work on their stroke rehabilitation device at the Schwada building on June 12, 2019. Photo by Deanna Dent/ASU Now
More Science and technology

Diagnosing data corruption
You are in your doctor’s office for your annual physical and you notice the change. This year, your doctor no longer has your health history in five-inch stack of paperwork fastened together with…
Large-scale study reveals true impact of ASU VR lab on science education
Students at Arizona State University love the Dreamscape Learn virtual reality biology experiences, and the intense engagement it creates is leading to higher grades and more persistence for biology…

ASU-led space telescope is ready to fly
The Star Planet Activity Research CubeSat, or SPARCS, a small space telescope that will monitor the flares and sunspot activity of low-mass stars, has now passed its pre-shipment review by NASA.…