Essential nutrient may help fight Alzheimer’s across generations

Mice with Alzheimer’s-like symptoms receiving supplemental levels of choline in the womb improved their spatial memory. A second generation bred from these choline-treated mice also showed improved spatial memory, suggesting epigenetic changes in genes. Choline acts to reduce harmful levels of the amino acid homocysteine, converting it to the beneficial chemical methionine. Graphic by Shireen Dooling
In a new study, researchers at the Biodesign Institute explore a safe and simple treatment for one of the most devastating and perplexing afflictions: Alzheimer’s disease.
Lead authors Ramon Velazquez and Salvatore Oddo, along with their colleagues in the ASU-Banner Neurodegenerative Disease Research Center, investigated the effects of choline, an important nutrient that may hold promise in the war against the memory-stealing disorder.
The study focuses on mice bred to display Alzheimer’s-like symptoms. Results demonstrate that when these mice are given high choline in their diet, their offspring show improvements in spatial memory, compared with those receiving a normal choline regimen in the womb.
Remarkably, the beneficial effects of choline supplementation appear to be transgenerational, not only protecting mice receiving choline supplementation during gestation and lactation, but also the subsequent offspring of these mice.
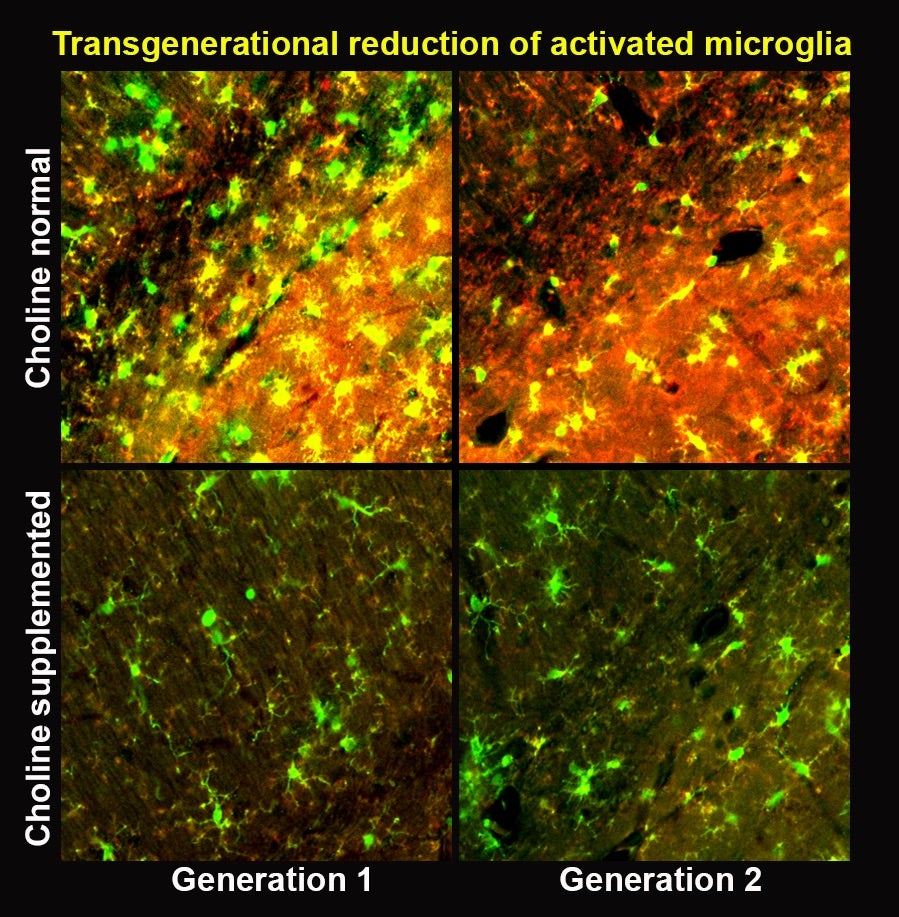
While this second generation received no direct choline supplementation, they nevertheless reaped the benefits of treatment, likely due to inherited modifications in their genes. The second generation also showed reduction in activated microglia.
The exploration of such epigenetic alterations may further exciting new avenues of research and suggest ways of treating a broad range of transgenerational afflictions, including fetal alcohol syndrome and obesity.
Supplementing the brain
Choline acts to protect the brain from Alzheimer’s disease in at least two ways, both of which are explored in the new study. First, choline reduces levels of homocysteine‚ an amino acid that can act as a potent neurotoxin, contributing to the hallmarks of Alzheimer’s disease: neurodegeneration and the formation of amyloid plaques.
Activated microglia, cells responsible for clearing debris from the brain, can cause inflammation and lead to neuronal death in Alzheimer's disease. The graphic shows the reduction of activated microglia when choline is given to prenatal mice.
Homocysteine is known to double the risk of developing Alzheimer’s disease and is found in elevated levels in patients with Alzheimer’s disease. Choline performs a chemical transformation, converting the harmful homocysteine into the helpful chemical methionine.
Secondly, choline supplementation reduces the activation of microglia — cells responsible for clearing away debris in the brain. While their housekeeping functions are essential to brain health, activated microglia can get out of control, as they typically do during Alzheimer’s disease. Over-activation of microglia causes brain inflammation and can eventually lead to neuronal death. Choline supplementation reduces the activation of microglia, offering further protection from the ravages of Alzheimer’s disease.
The findings appear in the current issue of the Nature journal Molecular Psychiatry. The ASU-Banner Neurodegenerative Disease Research Center researchers were joined by co-authors from the Translational Genomics Research Institute in Phoenix. (Oddo is also a researcher with ASU’s School of Life Sciences.)
Salvatore Oddo, a lead author of the new study, is a researcher in the ASU-Banner Neurodegenerative Disease Research Center and associate professor in ASU's School of Life Sciences.
Unremitting devastation
Alzheimer’s disease is now believed to begin its path of destruction in the brain decades before the onset of clinical symptoms. Once diagnosed, the disease is invariably fatal, shutting down one vital system after another. Mental decline is relentless, with patients experiencing a range of symptoms that may include confusion, disorientation, delusions, forgetfulness, aggression, agitation and progressive loss of motor control.
The disease is poised to afflict 13.5 million people in the U.S. alone by midcentury if nothing is done to address the disease. The staggering costs of Alzheimer’s are projected to exceed $20 trillion in the next 40 years. Developing effective treatments rooted in a more thorough understanding of this complex disease is one of the most daunting challenges facing modern medicine and the global health care infrastructure.
Altered states
Research into the origins of Alzheimer’s disease strongly suggests that a great variety of factors are at play. While advancing age remains the greatest risk factor, other hazards that have been implicated in the disease include genetic predisposition and lifestyle.
To this end, studies suggest that diet can have a significant effect in increasing or lowering the risk of cognitive decline, and the risks may be transmitted across generations. A classic case is known as the Dutch Hunger Winter — a severe famine in 1944-45 that affected pregnant women and their offspring.
When a recent study examined the adult health records of those born in the Netherlands during this period, results suggested that the severe dietary deprivation endured by the mothers of these children heightened the occurrence of obesity, above-average LDL cholesterol and, intriguingly, schizophrenia in their offspring. Mortality after 68 years of age increased by 10 percent in this population. It is believed that these adverse health effects occur as a result of the silencing of genes in unborn children. These health-related genes remain silenced throughout life, leading to poor health outcomes.
On a more hopeful note, a healthy diet has been shown to offer protection from diseases, including cancer and Alzheimer’s disease. Patients following a Mediterranean diet for 4.5 years lowered their risk of Alzheimer’s disease by 54 percent in one study. Another study pointed to the effects of a Mediterranean diet rich in fruits and vegetables, whole grains, legumes and nuts, as well as fish and poultry in reducing the accumulation of Aβ-amyloid, the protein responsible for plaque formation.
Ramon Velasquez, a lead author of the new study, is a researcher in the ASU-Banner Neurodegenerative Disease Research Center.
Effects of choline
Choline is a vitamin-like essential nutrient that is naturally present in some foods and also available as a dietary supplement. It is a source of methyl groups needed for many steps in metabolism. All plant and animal cells require choline to maintain their structural integrity.
Choline is used by the body to produce acetylcholine, an important neurotransmitter essential for brain and nervous system functions including memory, muscle control and mood. Choline also plays a vital role in regulating gene expression.
It has long been recognized that choline is particularly important in early brain development. Pregnant women are advised to maintain choline levels of 550 mg per day for the health of their developing fetus.
“There’s a twofold problem with this,” lead author Velazquez said. “Studies have shown that about 90 percent of women don’t even meet that requirement. Choline deficits are associated with failure in developing fetuses to fully meet expected milestones like walking and babbling. But we show that even if you have the recommended amount, supplementing with more in a mouse model gives even greater benefit.”
Indeed, when the Alzheimer’s study mice received supplemental choline in their diet, their offspring showed significant improvements in spatial memory. Subsequent examination confirmed the epigenetic alterations induced by choline supplementation. Modified genes associated with microglial activation and brain inflammation, and reduced levels of homocysteine resulted in the observed performance improvements in spatial memory tasks.
Due to the epigenetic modifications induced by choline, the improvements carried over to the offspring of mice receiving supplemental choline in the womb.
“We found that early choline supplementation decreased homocysteine while increasing methionine, suggesting that high choline levels convert homocysteine to methionine,” Velazquez said. “This conversion happens thanks to an enzyme known as betaine-homocysteine methyltransferase (BMHT). We found that choline supplementation increased the production of BMHT in two generations of mice”
The study’s significance is twofold, establishing beneficial effects from nutrient supplementation in successive generations and proposing epigenetic mechanisms to account for the reduction of Alzheimer’s disease memory deficit in mice.
“No one has ever shown transgenerational benefits of choline supplementation,” Velazquez said. “That’s what is novel about our work.”
Choline is an attractive candidate for treatment of Alzheimer’s disease as it is considered a very safe alternative, compared with many pharmaceuticals. The authors note that it takes about nine times the recommended daily dose of choline to produce harmful side effects.
Future work will explore the effects on Alzheimer’s disease of choline administered in adult rather than fetal mice. The authors stress, however, that while results in mice are promising, a controlled clinical trial in humans will ultimately determine the effectiveness of choline as a new weapon in the fight against Alzheimer’s disease.
More Health and medicine
College of Health Solutions program doing its part during Salute to Service
It wasn’t always easy for Marine veteran Chuck Hale when he first returned to civilian life. But he’ll never forget the help he…

What makes human culture unique?
Why is human culture — the shared body of knowledge passed down across generations — so much more powerful than animal cultures?“…

ASU honors students work on HPV research as part of Barrett College's largest-ever group thesis
Not every undergraduate student comes across the opportunity to do research as part of a team. Even fewer have had the chance to…