Your car won’t start, so you take it to a mechanic. They check the ignition, starter, timing belt, spark plugs, anything that might give a clue why the car won’t start.
If you took the car to an engineer, they would ask why is this model vulnerable to this problem? Is it a manufacturing defect? Was it never intended to be driven in a desert climate? Were there bad engineering decisions in the design?
The mechanic is modern medicine. The engineer is evolutionary medicine. And that is how Randy Nesse, founder of the field, elegantly explains it.
“It’s not why one person gets sick,” said Nesse, founding director of Arizona State University’s Center for Evolution and Medicine. “It’s why we all are vulnerable.”
Also called Darwinian medicine, it’s the application of modern evolutionary theory to understanding health and disease. The goal is to understand why people get sick, not simply how they get sick. Why are birth canals so narrow? Why can’t our bodies kill off every cancer cell?
“The big impact of this field is not in telling doctors a different way to practice medicine directly,” said Nesse, who is a professor in ASU's School of Life Sciences. “It’s on encouraging them to talk to patients in different ways, and encouraging researchers to ask entirely new questions. How can we prevent antibiotic resistance instead of just inventing new drugs all the time?”
Humans aren’t alone in this. Koala bears get cancer. Dragonflies can become obese. Flamingos can have heart attacks. Animals share most medical and psychiatric issues with our species, but physicians and veterinarians rarely consult with one another.
How human and animal common denominators can be used to diagnose, treat and heal all species is called zoobiquity. It’s the subject of a Darwin Day lecture, free and open to the public, sponsored by the Center of Evolution and Medicine on Thursday called “Not Uniquely Human.”
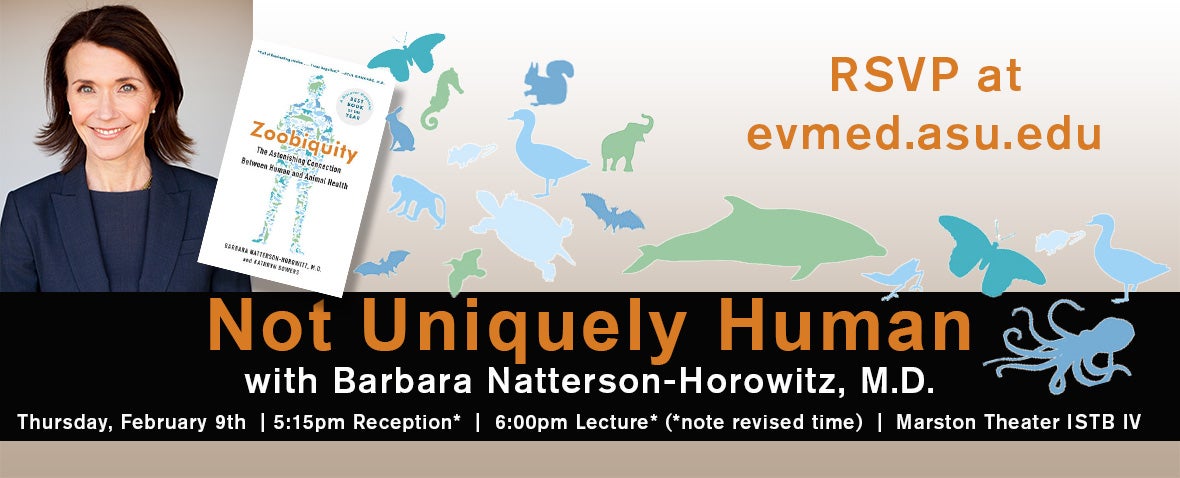
Dr. Barbara Natterson-Horowitz, author of "Zoobiquity: The Astonishing Connection Between Human and Animal Health," will explain the concept in Tempe on Thursday.
“Basically, it’s human medicine and veterinary medicine are the same, if you look at it from an evolutionary medicine viewpoint,” Nesse said.
The speaker will be Dr. Barbara Natterson-Horowitz, professor of medicine in the Division of Cardiology at the David Geffen School of Medicine at UCLA and adjunct professor in the UCLA Department of Ecology and Evolutionary Biology. Natterson-Horowitz is the author of “Zoobiquity: The Astonishing Connection Between Human and Animal Health.”
“I started really realizing that the essential vulnerability we have to disease is quite ancient,” Natterson-Horowitz said. “They are not unique to modern times or our own species.”
It’s a shift in how we think about human disease, she said.
“Evolutionary biology is as fundamental to medicine as mathematics is to engineering,” she said. “Most physicians have not been trained in evolutionary biology. That’s changing. There are a number of ways this approach can help health in humans and animals.”
There is a form of stress-induced heart disease called stress cardiomyopathy. By looking across species, Natterson-Horowitz learned that there are many wild animals that die from heart stress during capture. Susceptibility to this varies across taxa. Groundhogs are pretty chill, but pikas can die of sudden fright. She did a study of reports of the same thing in ungulates like giraffes, camels and deer and saw differences in vulnerability.
Has natural selection resulted in certain species of ungulates having enhanced resistance? Why, and how? Can that mechanism help us understand sudden stress death in human beings? This is where medicine and ecology and evolutionary bio intersect.
It’s often said a cure for disease could be found in an undiscovered plant in the Amazon. Through the lens of zoobiquity, the same could be said of animals roaming the Serengeti.
“We need to know about the lives of these animals,” Natterson-Horowitz said. “In my mind, this speaks to a very important conservation message. … Embedded in the world’s biodiversity could be the solution to some of our health questions. It’s fundamentally a call for conservation.”
One principle of evolutionary medicine that everything is a trade-off. Too much acid? Bad. Not enough acid? Bad? Too tall? Bad. Too short? Bad. But bad things can be good.
“People think anxiety is a bad thing, but they don’t think about the people who don’t have enough anxiety,” Nesse said. “They’re all dead. One of the most interesting things about anxiety disorders is a calculation I’ve done trying to figure out why do so many of us have so much excess anxiety.”
He pointed to the smoke detector principle. If you’re out in the African savannah, and there might be a lion behind that rock, should you run away? Running away is going to cost 100 calories. Not running away, if there’s no lion there, would save 100 calories. Not running away, if there is a lion there, might cost you 100,000 calories. The ratio there is 100 to 100,000. So, how loud does the noise behind the rock have to be before you should run like hell? Any noise that’s loud enough to indicate a lion is there with a greater probability of 1 in 1,000 means that you should run away, even though 999 times there’s no lion.
In this case anxiety is healthy. “It’s normal,” Nesse said. “It’s useful. The cost of a false alarm is low. The cost of not running away if there’s a lion there is death.”
Doctors might treat a diagnosis of anxiety with medication. Evolutionary medicine offers a different principle for guiding decisions about when to use drugs like that.
It has profound implications for psychiatry. Winston Churchill was plagued by a depression he called his “black dog.”
“Why do we have a capacity for low mood and the blues?” Nesse said. “We all do. Under certain circumstances we get pessimistic. Why? It turns out that every species has some way to regulate its motivation and spend more effort at times when things pay off. When nothing pays off, the best thing to do is nothing. In our lives that’s more complicated than it is for a bird trying to find seeds.”
Top photo: Randy Nesse, an evolutionary biologist and psychiatrist and founding director of the Center for Evolution and Medicine at Arizona State University, says the big impact of his field is in encouraging doctors "to talk to patients in different ways, and encouraging researchers to ask entirely new questions." Photo by Deanna Dent/ASU Now
More Science and technology

ASU postdoctoral researcher leads initiative to support graduate student mental health
Olivia Davis had firsthand experience with anxiety and OCD before she entered grad school. Then, during the pandemic and as a result of the growing pressures of the graduate school environment, she…
ASU graduate student researching interplay between family dynamics, ADHD
The symptoms of attention deficit hyperactivity disorder (ADHD) — which include daydreaming, making careless mistakes or taking risks, having a hard time resisting temptation, difficulty getting…

Will this antibiotic work? ASU scientists develop rapid bacterial tests
Bacteria multiply at an astonishing rate, sometimes doubling in number in under four minutes. Imagine a doctor faced with a patient showing severe signs of infection. As they sift through test…
