The path from roundworm genes to curing cancer isn’t an easy one.
But a handful of students and faculty at Arizona State University are joining forces to increase our understanding of how small biological changes in genes can influence the development, diagnosis and treatment of cancer.
Two faculty laboratories within ASU’s Virginia G. Piper Center for Personalized Diagnostics — and the students who work there — are fusing fundamental science with clinical research to create more effective diagnostic and treatment options for multiple types of cancer.
“Neither of our labs could do this on our own,” said Dr. Karen Anderson, medical oncologist at Mayo Clinic Arizona and associate professor in the Biodesign Institute and School of Life Sciences. “We have the potential of thinking about the problem in a different way, and I think that’s really important.”
The collaborative effort and shift in thinking allow students like Justin Wolter, who’s pursuing a Doctor of Philosophy in molecular and cellular biology, to identify how biological mechanisms play a role in cancer development and progression.
Bianca Varda, an undergraduate in Anderson’s lab, has been utilizing Wolter’s expertise in molecular biology to develop new ways to activate the immune system to fight a specific strain of HPV before it leads to oropharyngeal cancer, which affects tissues in the throat such as the tongue and tonsils.
Their research, along with other lab initiatives, is part of finding innovative cures for diseases from some of the most unexpected places.
“Maintaining a balance between basic and translational research is really important to allow for fundamental discoveries that can be applied to human health,” said Wolter.
Worm to human genes
Wolter is on a team of researchers in assistant professor Marco Mangone’s lab who have been conducting experiments — using the roundworm as a model organism — to explore what key roles genes play in producing a variety of complex life forms, from fruit flies, to mice, to humans. The newfound understanding of this tiny worm’s genetics can then be translated to human cell lines when trying to determine how genes are broken in diseases.
“Cancer is an incredible model because essentially it’s just cells growing and dividing,” said Wolter. “The exact opposite of what they should be doing.”
Under the mentorship of Mangone, Wolter’s research has focused on two genes, known as microRNAs, that are relevant to breast cancer prognosis and progression. One gene limits tumor formation by slowing cell division and growth. The other gene triggers the transition from a benign tumor to the more aggressive metastatic form by allowing cells to break free and colonize at a new site in the body.
“What’s really interesting about these two genes is they’re tiny,” said Wolter. “How they regulate a large number of genes and give you such different behaviors, different phenotypes and different contributions to the disease is really unknown.”
Using evidence from the genomes of different animals, Wolter’s research aims to show how single mutations in these genes throughout the course of evolution can have an effect on human disease.
“There’s a lot of interest to study disease-relevant genes,” said Wolter. “So that’s a big motivational factor for me and our lab to try to look at ways we can modulate these genes or change when and where they’re expressed to combat some of the more severe forms of cancer.”
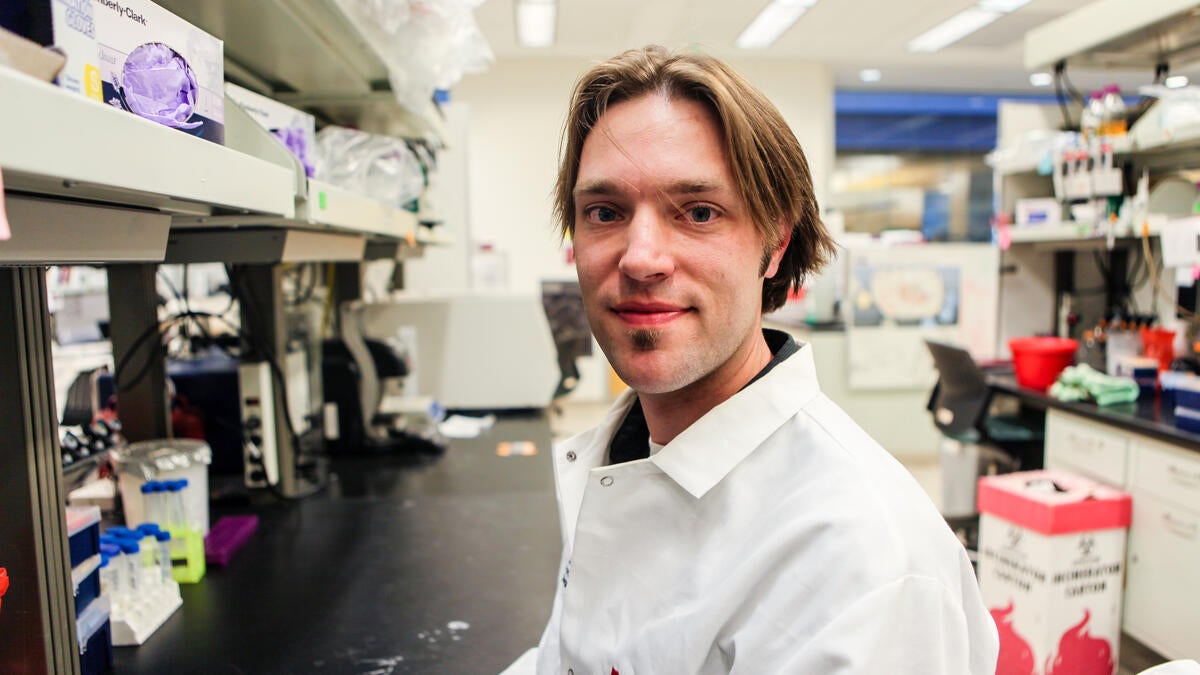
Two faculty laboratories within ASU’s Virginia G. Piper Center for Personalized Diagnostics — and the students who work there — are fusing fundamental science with clinical research to create more effective diagnostic and treatment options for multiple types of cancer. Photo by Esly Diaz/ASU
Translating basic research into cures
Anderson, who also serves as a faculty member on Wolter’s graduate committee, utilizes these types of findings from basic research to develop cancer detection and treatment options through immunology.
Researchers in Anderson’s lab have been studying how our immune systems can detect cancers based on small changes in our cells. Differences in proteins and other changes create biomarkers for different cancer types, which serve as another method for early disease detection.
“The real question right now is how early can we find these cancers,” said Anderson.
By measuring biomarkers in the blood specific to breast cancer, researchers in her lab have been working to develop a blood test that can be used with mammograms to find cancer earlier.
“We have a number of blood test-based biomarkers that are currently under investigation to determine how useful they might be clinically,” said Anderson.
Anderson’s team has also been examining how to change and activate the immune system to fight off cancer — a project undergraduate Bianca Varda has been working on solving for HPV-related cancers.
Varda, a biological sciences major in the School of Life Sciences and Barrett, the Honors College, has been studying how the immune system interacts with HPV 16 — one of a dozen types of high-risk HPVs that cause nearly 5 percent of all cancers worldwide. She has been engineering a system that will help measure and initiate an immune response to detect head, neck and cervical cancer.
HPV 16, along with HPV 18, is responsible for most HPV-caused cancers, including cervical, throat and anal cancers. In the U.S., more than 50 percent of cancer diagnoses in oropharynx (the middle part of the throat) are linked to HPV 16, while HPV 16 and 18 cause nearly 70 percent of all cervical cancer cases.
Varda’s work centers on activating the immune system by finding specific cellular protein, or peptide, sequences that trigger antigens, a molecule responsible for creating an immune response. Specifically, she’s looking to activate T cells, a type of white blood cell that assists in an active immune response.
“Right now we’re working on identifying specific peptide sequences that correspond to the HPV 16 antigens,” said Varda. “So we can stimulate T cells … and essentially use the immune system to fight off the cancer.”
“We need good researchers. They’re the future of our world.”
— Dawn Carson Senger, co-creator of the Carson Senger New American University Scholarship
Varda hopes her research will lead to the development of treatments for the millions of people infected with HPV, preventing the progression of HPV 16-related cancers.
“I got lucky to find a lab that’s doing something really interesting,” said Varda. “[But] without scholarships I wouldn’t be in the lab as much or at all.”
Funding student research experiences
Student research has been a long-time priority for two different families who have seen the devastating effects of cancer.
Dawn Carson Senger and Erston Senger, donors for Varda’s scholarship, established the Carson Senger New American University Scholarship to support a student with an interest in medical, biomedical or cancer research.
“We need good researchers,” said Carson Senger. “They’re the future of our world.”
John and Rose Maher, donors for Wolter’s scholarship, created the Maher Alumni Scholarship to support a graduate student pursuing cancer research while at ASU.
Affected by the loss of a friend and family member to the disease, John Maher said this was their answer to finding a cure for cancer and defeating it.
“Every single person we’ve sponsored with our scholarship has done a superb job with research, and Justin is continuing that terrific tradition,” said ASU alumnus John Maher. “He’s willing to work hard and get it done.”
Next steps
While the discovery of a simple cure for cancer is still underway, the research is already having a positive impact on Wolter and Varda.
After completing his doctorate, Wolter said he wants to stay in academia and run a lab at a university to continue his research in gene regulation and developmental biology.
Similarly, Varda wants to continue her research as a physician and is applying to medical school this spring.
“I definitely plan to use and apply [my research] hopefully in the medical world,” said Varda. “I think it’s really important to understand the science behind the medicine you’re practicing.”
The unyielding motivation and scientific curiosity of students in the lab are part of what makes the work worth it, said Anderson.
“I like being able to educate the next generation of scientists,” she said. “They will solve this, I believe.”
This story was published in the College of Liberal Arts and Sciences Magazine as part of the spring/summer 2016 issue.
Top photo: Graduate student Justin Wolter in professor Marco Magone's lab within ASU’s Virginia G. Piper Center for Personalized Diagnostics. Photo by Esly Diaz/ASU
More Science and technology
ASU graduate student researching interplay between family dynamics, ADHD
The symptoms of attention deficit hyperactivity disorder (ADHD) — which include daydreaming, making careless mistakes or taking risks, having a hard time resisting temptation, difficulty getting…

Will this antibiotic work? ASU scientists develop rapid bacterial tests
Bacteria multiply at an astonishing rate, sometimes doubling in number in under four minutes. Imagine a doctor faced with a patient showing severe signs of infection. As they sift through test…

ASU researcher part of team discovering ways to fight drug-resistant bacteria
A new study published in the Science Advances journal featuring Arizona State University researchers has found vulnerabilities in certain strains of bacteria that are antibiotic resistant, just…