Evolving the framework of cancer theory

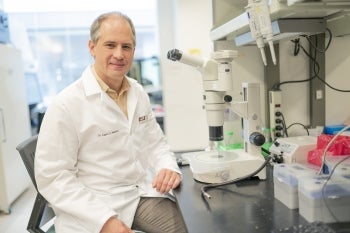
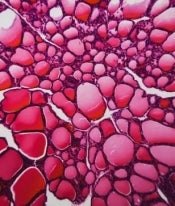
A recent review by Carlo Maley, a researcher at Arizona State University, and Lucie Laplane from the University of Paris Pantheon-Sorbonne critiques the dominant theory of cancer evolution. The authors discuss both the practical and theoretical limitations of the clonal model of cancer evolution and suggest ways to enhance its relevance and accuracy. Graphic by Jason Drees
Cancer cells are driven by the same imperative guiding all living things: to grow, survive and reproduce. Although cancer’s evolutionary underpinnings have been recognized since the 1950s, clinicians have been slow to apply the lessons of evolution to the fight against this deadly disease, which remains the second-leading cause of death, claiming 9.7 million lives worldwide in 2022.
A new review by Arizona State University researcher Carlo Maley and Lucie Laplane from the University of Paris Pantheon-Sorbonne examines the prevailing theory of cancer evolution. The authors highlight both practical and theoretical limitations of the clonal model of cancer evolution and propose areas for improving the model’s relevance and accuracy.
The study suggests that the model could be improved by acknowledging that cancer cells inherit not only genetic mutations but also other traits that allow them to rapidly adapt to their environment — even without genetic alterations. Cancer cells are highly responsive to their surrounding environment, which can promote or suppress their growth. Further, cancer evolution often follows complex dynamics, leading to tangled and unpredictable growth patterns.
Cancer biologists have traditionally defined a "clone" as a group of cells descending from a single ancestor cell and sharing the same genetic makeup. But cancer cells mutate so fast that no two cells have the same genetic makeup. The study proposes replacing the concept of a clone with a focus on the cell genealogies that record the history and define the structure of the cells in a tumor.
The value of an effective model lies in its ability to explain how and why cancers evolve and respond to therapy. By refining the clonal evolution model, the study paves the way for more effective cancer therapies that consider the full complexity of cancer cell evolution.
The research appears in the current issue of the journal Nature Reviews Cancer.
“Evolution is such a powerful idea that when we apply it to the cells in our bodies, it explains how we get cancer and why it is so hard to cure. But, like everything in the real world, it’s complicated,” Maley says. “We set out to address the complications that people have pointed out and show how they can be integrated into our theory of how cancer works.”
Maley is a researcher in the Biodesign Center for Biocomputing, Security and Society, director of the Arizona Cancer Evolution Center and professor with ASU’s School of Life Sciences.
His collaborator, Lucie Laplane, visited ASU for the research project, thanks to the generous support of the Center for Biology and Society and a grant from the McDonnell Foundation.
Cancer beyond mutation
The clonal evolution theory of cancer suggests that cancer begins from a single cell that undergoes mutations, enabling it to grow and divide faster than normal cells. As this cell divides, some of its offspring may gain additional mutations that provide even greater advantages in survival and growth. Over time, this process leads to a population of cancer cells that are very diverse but driven by those that are most fit for survival and reproduce in their environment. This theory helps explain why cancers can be so challenging to treat — they continuously evolve, making them adaptable to various therapies and environments.
The latest research in cancer
From diagnosis and treatment to prevention, the Biodesign Institute takes a comprehensive approach to cancer research. Learn more.
To address these issues, the researchers explore the limits of the current evolutionary cancer theory. A key challenge is expanding this theory to encompass all the ways cancer evolves, including inheritance of more than just genes when cells divide and genetic material exchange among cells, as well as developing better methods to identify and track cancer cell variations.
Traditionally, it has been assumed that the DNA of cancer cells largely determines their behavior and progression. This includes how they grow, spread and respond to treatments. The study challenges this view, highlighting other factors such as the influence of a cell's surrounding environment and epigenetic changes — chemical modifications that alter gene expression without changing the genetic sequence.
Another assumption is that the development of cancer can be traced like a tree, from one main ancestor cell branching out into all the cancer cells found in a tumor. That model implies a neat, predictable pattern of cancer growth. However, the study suggests this is not always the case. Cancer cells can merge (through cell fusion) or acquire traits from other cells. This could make the growth pattern of cancers more complex, resembling more of a network with multiple influences and paths.
Further, while clonal evolution was initially considered a continuous, gradual process, it has been shown to occur during stasis, gradual change, or in sudden, punctuated bursts.
An evolving portrait of cancer
The clonal evolution model has already brought about a significant shift in how we view cancer, highlighting the disease’s profoundly dynamic nature. This shift in perspective has helped discredit the search for a single "magic bullet" treatment and prompted changes in both research and treatment approaches.
Although the clinical impact of evolutionary theory has been limited so far, a range of evolutionary strategies for treatment has shown encouraging results, such as adaptive therapy, which can lead to dramatic improvements in time to progression and overall survival.
Understanding the multifaceted nature of cancer evolution is critical for developing more effective treatments. The study suggests that targeting not only genetic mutations but also epigenetic changes and interactions with the surrounding cell environment could improve treatment outcomes.
By refining the clonal evolution model, the study paves the way for more effective cancer therapies that consider the full complexity of cancer cell evolution.
More Science and technology

Breakthrough copper alloy achieves unprecedented high-temperature performance
A team of researchers from Arizona State University, the U.S. Army Research Laboratory, Lehigh University and Louisiana State University has developed a groundbreaking high-temperature copper alloy…

4 ASU researchers named senior members of the National Academy of Inventors
The National Academy of Inventors recently named four Arizona State University researchers as senior members to the prestigious organization.Professor Qiang Chen and associate professors Matthew…

Transforming Arizona’s highways for a smoother drive
Imagine you’re driving down a smooth stretch of road. Your tires have firm traction. There are no potholes you need to swerve to avoid. Your suspension feels responsive. You’re relaxed and focused on…