Stressed, exhausted and sitting in a hospital waiting room, the last thing anyone wants to do is spend half an hour filling out paperwork. Yet that is the first task patients and caregivers are saddled with during a hospital visit.
This not only takes away precious time that could be spent with the physician, it creates a burden for the doctor as well. She has to scramble to read through forms moments before she walks in the room. After the visit, she must enter them into the electronic medical record along with her own notes.
Currently, doctors spend around two hours of their time on electronic medical records for every one hour of face time with patients, according to a study by the Annals of Family Medicine.
To improve this process, Phoenix Children’s Hospital — one of the largest pediatric health care systems in the U.S. — partnered with Arizona State University to form a Practice Lab. Practice Labs bring together interdisciplinary teams of students to help companies creatively solve pressing issues.
The Phoenix Children’s team is creating a dynamic web app that allows patients to submit their information before an appointment and then enters that information directly into the health system’s records.
“We're reducing time that providers spend on collecting data, which means they can serve more patients, which means that people get more access to health care. There's some noble pursuit that we are achieving here,” said Chase Adams, co-principal investigator on the project and assistant director of the ASU Luminosity Lab, which develops student teams for Practice Labs.
“It was undoubtedly a great opportunity to bring new energy and new insight,” said David Higginson, the executive vice president and chief operating officer of Phoenix Children’s. “It was time to come up with a solution to an old, ongoing pain point that most health care systems face.”
“It’s an exposure to the outside world,” said Nikhil Agarwal, a computer science master’s degree student with the project. “We get to interact with professionals and understand what problems they are facing and whether we could make their lives easier.”
Diagnosing the problem
The medical staff at Phoenix Children’s have long struggled with issues related to physical patient forms. Typically, the health system needs to collect three types of information from a patient: past history, such as prior surgeries or illnesses; family history, such as hereditary diseases; and social history, such as education and income.
“We felt that the patient family should have the opportunity to input this kind of background data when they have time at home, rather than in their doctor's office,” said Vinay Vaidya, senior vice president and chief medical information officer at Phoenix Children’s, who collaborated with the Practice Lab.
The hospital and Practice Lab team decided to focus on collecting family history as the first step in developing their app.
To better understand how health care professionals go about doing that, the students met with genetic counselors, who evaluate and advise families on genetic disorders. The counselors conducted mock interview sessions that allowed the students to see how they might improve the process and learn where patients typically have questions.
One of the team’s biggest takeaways was gaining experience working in an interdisciplinary group, much like they would in an industry setting. Communication has been key, they say, to ensuring that their individual work comes together cohesively.
Prescribing a simpler solution
The Practice Lab’s web app is a serious upgrade to the typical paper form. One of the main differences is that it only asks patients for information relevant to their hospital visit. For example, if a patient is at the hospital for a heart-related problem, the app will not ask questions about a family history of vision problems.
The app also saves the patient’s information for future visits, so there is no need to answer the same questions over and over. Instead, the patient can update information that has changed, which will allow the doctor to track the patient’s health over time.
“This benefits both the doctor and the patient,” Agarwal said. “The patient doesn't spend time filling data that he has actually already filled, and the doctor doesn't waste time looking at excess data.”
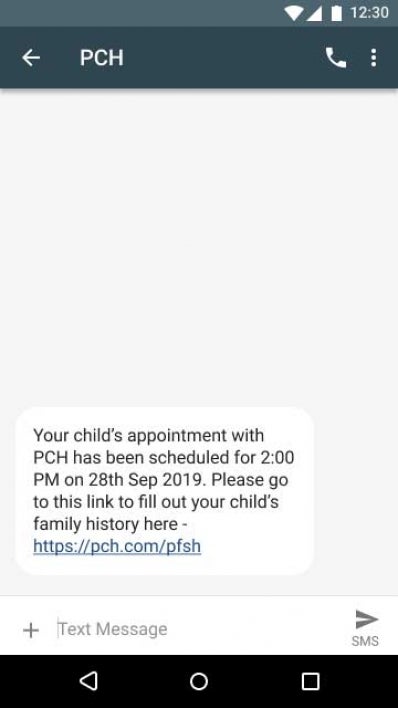
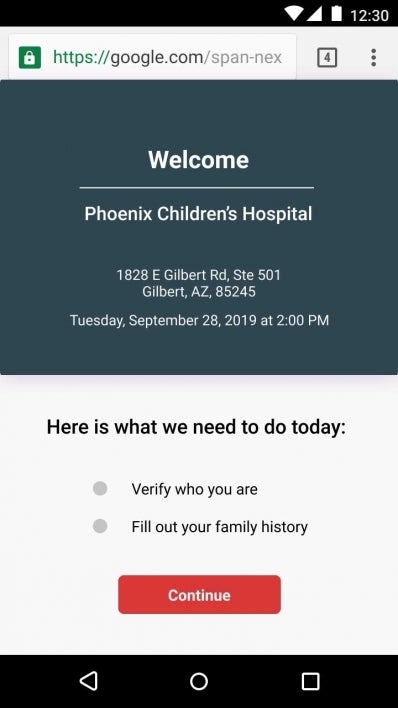
The app will work like this: A few weeks before an appointment, patients will get a text message from Phoenix Children’s with a link that will prompt them for authentication before taking them to the web form.
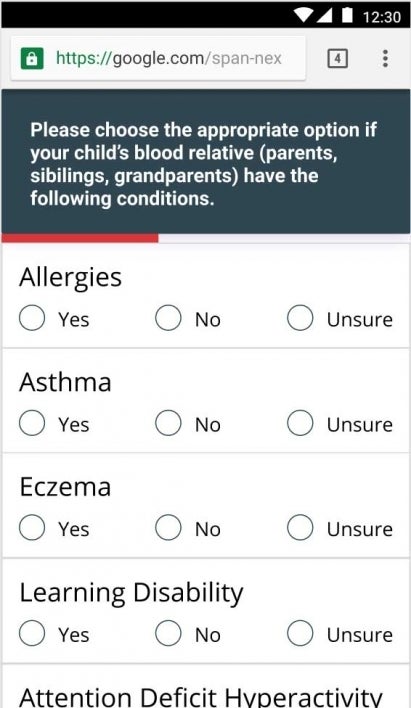
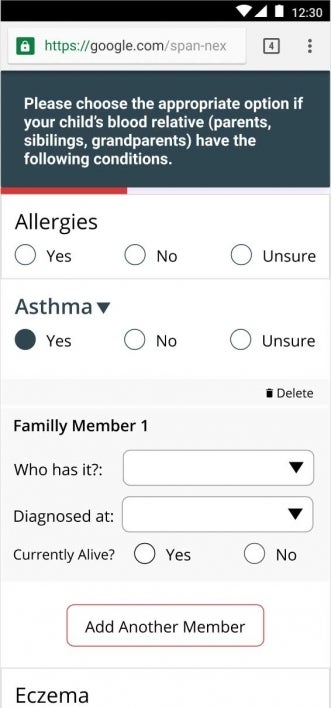
Once in the app, patients will be asked questions related to their appointment. Answers are in a simple “yes, no, unsure” format. Depending on how patients answer, the app will customize the questions that follow.
Patients can also leave and return to the form if, for example, they need to ask family members about their medical history.
The project team hopes that the ease of use will free patients to fill in more complete information than a paper form, or doctors’ notes, would allow.
“A lot of the patients that come in aren't necessarily tech savvy, so to make sure that it was as simple as possible was the biggest priority,” said Kusum Ijari, a human systems engineering master’s degree student.

ASU student Kusum Ijari (center) goes over the app’s design with fellow team members Nikhil Agarwal (left), Rakshith Subramanyam (bottom right) and Siddarth Madan Kumar (upper right). Photo credit: Andy DeLisle
A positive prognosis for the future
The Practice Lab’s user testing suggests they were successful. The team asked parents who worked in the Luminosity Lab to fill out the web form with their children’s family medical history. The test subjects were able to complete the form in an average of just three minutes.
The team also made an effort to keep the coding for this app clean and modular, like Lego blocks, to enable add-ons of other potential features in the future. Those could include graphs or medical family trees using patient data; a Spanish version; or expansion of the app to gather patients’ past and social histories.
The project entered a new phase at the end of October, when the team handed their code over to Phoenix Children’s for further testing and refining.
The health system will ensure that the app meets the industry’s rigorous security standards and offers a seamless user experience before launch. Higginson says he hopes to begin pilot testing in the first or second quarter of 2020.
The app represents the latest wave in a growing trend of integrating technology in health care. Now that doctors can interact through electronic medical records, the industry is ready for better virtual communication with patients.
People on both ends of the stethoscope will likely be more than happy to leave the clipboards, flower pens and lengthy forms behind in exchange for a few taps on the screens in their pockets.
If your organization is interested in forming a Practice Lab with ASU, please contact ASU’s Business Concierge at corporate@asu.edu for more information. Learn more about ways companies can partner with ASU.
Top photo: ASU students Rakshith Subramanyam (left) and Nikhil Agarwal (right) work on the web app. Photo credit: Andy DeLisle
More Science and technology

ASU postdoctoral researcher leads initiative to support graduate student mental health
Olivia Davis had firsthand experience with anxiety and OCD before she entered grad school. Then, during the pandemic and as a result of the growing pressures of the graduate school environment, she…
ASU graduate student researching interplay between family dynamics, ADHD
The symptoms of attention deficit hyperactivity disorder (ADHD) — which include daydreaming, making careless mistakes or taking risks, having a hard time resisting temptation, difficulty getting…

Will this antibiotic work? ASU scientists develop rapid bacterial tests
Bacteria multiply at an astonishing rate, sometimes doubling in number in under four minutes. Imagine a doctor faced with a patient showing severe signs of infection. As they sift through test…