ASU engineer working to develop disposable point-of-care sensor
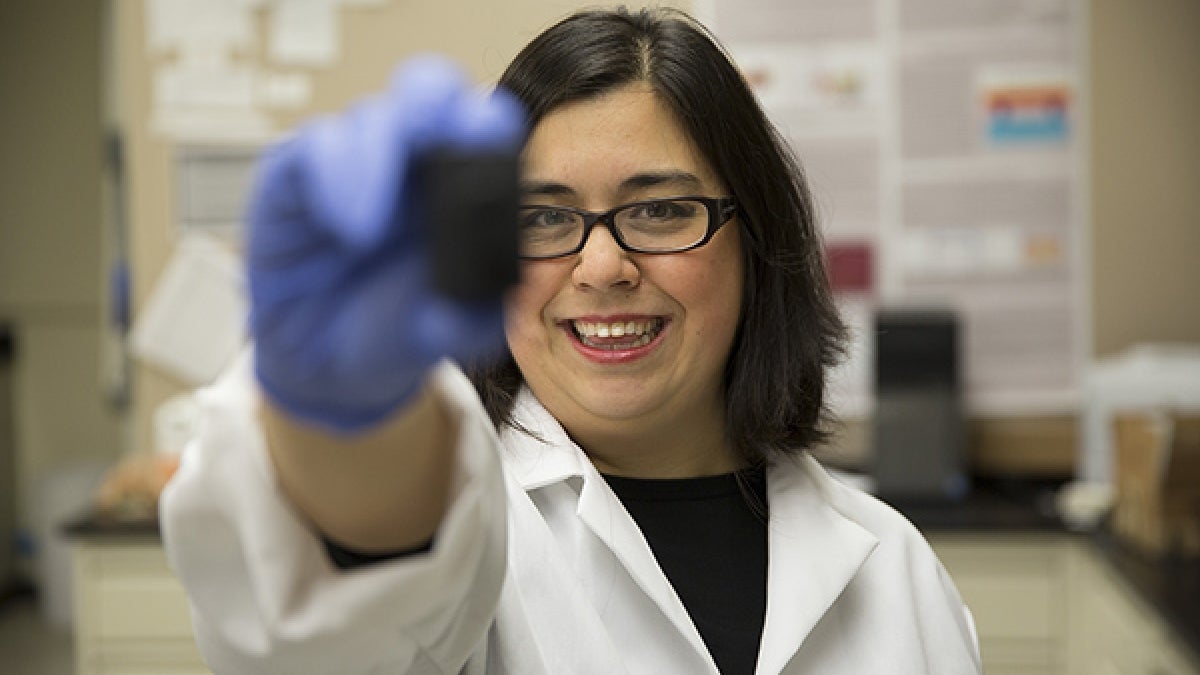
Associate Professor of electrical engineering Jennifer Blain Christen holds an early prototype of a point-of-care diagnostic tool, which samples biomarkers in sweat to provide an immediate look into a patient's health. Photo by Pete Zrioka/ASU
As an electrical engineer, Associate Professor Jennifer Blain Christen has spent a good portion of her career dabbling in different fields.
Her enthusiasm for exploring new and different ways of applying electrical engineering earned her the funding to leverage her expertise to create an innovative new diagnostic tool.
The project aims to develop a disposable, point-of-care biosensor for rapid diagnosis and health monitoring, supported by a four-year, $1.8 million Smart and Connected Health award from the National Science Foundation.
Working in conjunction with Arizona State University’s Flexible Display Center and Professor Karen Anderson of the Biodesign Institute and the School of Life Sciences, Blain Christen envisions a sweat-absorbing patch about the size of a nicotine or birth control patch with the ability to provide an immediate window into a patient’s health.
This is accomplished with a small screen within the patch, much like a miniature TV screen, which uses light to examine molecules within sweat. The screen projects light through the molecules, and the color of light that emerges indicates the presence or absence of disease.
An added benefit of this approach is that each pixel on the screen can look for different biomarkers, or measurable indicators that can be used to diagnose disease, to look for a variety of illnesses or health conditions.
Blain Christen, a faculty member in the Ira A. Fulton Schools of Engineering, also wants to enable these sensors to communicate with mobile devices, leveraging the computing power we all carry around with us in our smartphones.
“This way, it’s delegating diagnosis and monitoring to machines, so physicians and health-care professionals can dedicate their time to treatment,” she said.
In addition to saving time, designing the patch to communicate with ubiquitous mobile devices opens new possibilities beyond point-of-care applications.
“There’s a huge availability of these devices that are really powerful computers,” said Blain Christen, who envisions using that power to collect location data to aid in epidemiological studies.
As an example, she points to developing nations, where it can be difficult to determine the severity and spread of an illness. In countries with dispersed, remote populations, there aren’t adequate resources nor technology available to effectively collect data.
Using existing devices, patch data could be sent to a central location for further study and analysis, providing a holistic picture of a disease or infection.
“Everyone has a cellphone. In some cases, people have cellphones before indoor plumbing,” said Blain Christen. “Why not use that technology to collect the information for a centralized body? That way you empower people with information to do something about it.”
The patches are designed to be cheap and disposable; they can be used one time and then discarded — another positive for their use in the developing world.
“A lot of different electronics components have gotten smaller and cheaper, so we can put more advanced capabilities into this thing while making it smaller and still retain the same kind of cost point for the technology,” said Blain Christen.
Such affordable, disposable devices have a range of applications — for instance, use as a rapid screening device for people entering a country from a region afflicted by Zika virus, Ebola or dengue fever, so that infections can be detected before they spread.
In addition to curbing epidemics and quickly identifying disease, the patches are being developed with sustained diagnostics in mind. Blain Christen and Anderson collected sweat samples to measure stress biomarkers to aid in the development of timed spot sensors — sensors that collect data over a period of time.
“We can time sequence it, so we can look for the same molecule at specific times throughout the day using different pixels,” said Blain Christen. “You can imagine when you wake up, your stress levels are going to be different than after you’ve had your morning coffee or you go out for a job or you’re sitting in your office all day.”
The collaboration between Anderson and Blain Christen began about three years ago. Blain Christen, who did her post-doctoral studies in a clinical lab at Johns Hopkins University, has long been interested in biomedical devices. When she first started at ASU, the Biodesign Institute was one of her first stops, where she began looking for research collaboration opportunities.
After an emphatic response from Anderson, Blain Christen knew it was the beginning of a great working relationship.
“She has a unique perspective. Though she’s a physician with a background in medicine, she understands engineering well enough to know what is possible,” Blain Christen said of Anderson. “She sees how you could create something that isn't there now. She’s really great at identifying all the possible applications for technology in health care.”
Likewise, while Blain Christen’s work is based in electronics, it’s the application of her research to other areas that she finds the most rewarding.
“We have such rich availability of resources in electronics,” she said. “To be able to leverage that and bring that into a new field is really exciting. It’s so much fun to learn and experiment with my discipline in other fields.”
More Science and technology

Hack like you 'meme' it
What do pepperoni pizza, cat memes and an online dojo have in common?It turns out, these are all essential elements of a great…

ASU professor breeds new tomato variety, the 'Desert Dew'
In an era defined by climate volatility and resource scarcity, researchers are developing crops that can survive — and thrive —…

Science meets play: ASU researcher makes developmental science hands-on for families
On a Friday morning at the Edna Vihel Arts Center in Tempe, toddlers dip paint brushes into bright colors, decorating paper…

